Why Do I Have a Bust of William Arbuthnot Lane in My Office Waiting Room?
If you’ve ever sat in my waiting room and noticed the bronze bust of a serious-looking man, you may have wondered who he is. That man is Sir William Arbuthnot Lane — and he’s more than just a historical curiosity.
He’s also my great-great-grandfather.
The bust was given to me by my grandmother, his granddaughter. I keep it here not just as a family heirloom, but as a daily reminder of how medicine evolves — and how sometimes, even great innovations can be taken too far.
Lane and the Birth of Sterile Surgery
William Arbuthnot Lane (1856–1943) practiced at a time when surgery was still extraordinarily dangerous. Patients routinely died of infections after even the most minor procedures. In the late 19th century, Joseph Lister had introduced antiseptic surgery — spraying carbolic acid to kill bacteria that contaminated wounds during operations. It was groundbreaking but still imperfect.
Lane took things a major step further. Drawing on two scientific revolutions from continental Europe:
- Louis Pasteur’s germ theory (France), which proved that microscopic organisms caused infections;
- Ernst von Bergmann’s aseptic technique (Germany), which sterilized instruments and created fully sterile surgical fields;
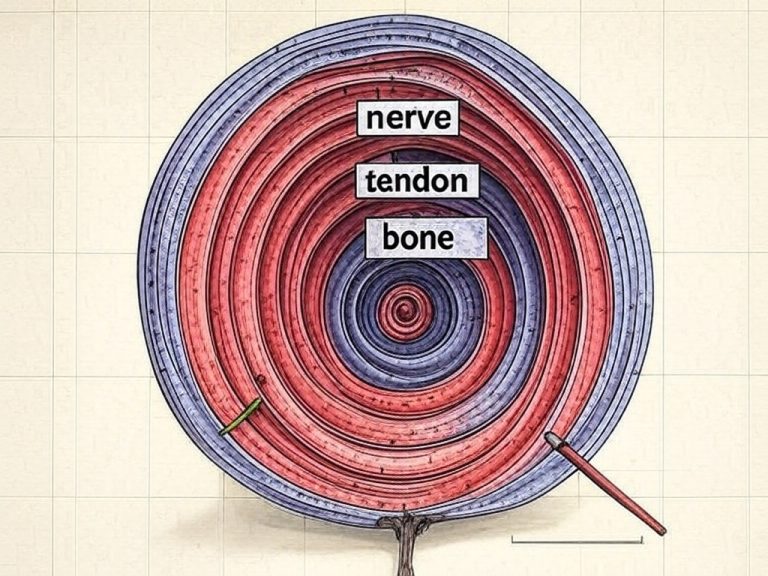
Lane pioneered the modern sterile operating room — abandoning antiseptics entirely and preventing contamination before it occurred. His success in achieving sterility allowed him to perform procedures that had been previously too dangerous, most notably the internal fixation of fractures using metal plates and screws. That work laid the foundation for much of modern orthopedic and trauma surgery.
The 20th Century: When Sterility Was a Lifesaver
Through the 20th century, sterile technique fueled incredible advances: neurosurgery, heart surgery, organ transplants, joint replacements — all required extraordinary levels of sterility to succeed. In these complex, high-risk fields, the operating room evolved into a kind of sterile cathedral: with positive pressure airflow, full surgical suits, and layers of infection control.
In these cases, Lane’s legacy remains absolutely vital. Infection in a joint implant or heart valve can be catastrophic, and the extreme sterility of modern ORs has saved countless lives.
The Problem: When “More Sterility” Becomes Overkill
But over time, something predictable happened: what began as vital patient protection eventually morphed into medical overkill. As American healthcare industrialized, the highly controlled, highly expensive operating room became the default setting for almost any procedure, regardless of the actual risk of infection.
Simple soft-tissue surgeries — like carpal tunnel releases, tendon repairs, many podiatry procedures, oral surgeries, and minor vascular procedures — are now routinely performed in full operating rooms, even though they could be done perfectly safely in simpler outpatient procedure rooms.
The result? Massive added costs to the system and to patients, with no real improvement in safety.
The Evidence Is Clear: Many Procedures Don’t Need Full OR Sterility
In recent years, many surgeons have been re-examining whether full OR sterility is necessary for every surgery — and the data are clear. For many minor surgeries, field sterility — meaning a properly prepped sterile field but without full OR infrastructure — is just as safe.
One of the leading voices is Dr. Don Lalonde, who pioneered a technique called WALANT: Wide Awake Local Anesthesia No Tourniquet. In a 2012 paper, he demonstrated that hand surgeries done under WALANT with field sterility had an infection rate of just 0.5% — identical to full OR sterility, but with less cost, less waste, and far greater patient comfort (Lalonde et al., 2012).
Building on this, my own 2024 study followed infection rates as I transitioned hand surgery cases from the hospital OR to a field-sterile office procedure room. The result? No significant change in infection rates despite eliminating the full OR environment (Clarkson, 2024).
Other studies echo these findings:
- A 2021 study of 265 upper extremity surgeries found a 0.37% infection rate using field sterility (Avoricani et al., 2021).
- A 2019 review found no added benefit from full OR features like laminar airflow, head covers, or specialized footwear for minor hand procedures (Yu et al., 2019).
In other words, once you’ve achieved “good enough” sterility, adding more complexity doesn’t improve safety — it only adds cost.

Why Lane Still Belongs in My Waiting Room
So why keep Lane’s bust here?
Not to glorify sterile excess — but to honor what his work truly represents: courageous scientific evolution. He wasn’t afraid to challenge the orthodoxy of his day and make surgery safer based on new science. But the best way we can honor his legacy today is to follow that same principle — to keep questioning, to keep adapting, and to recognize when further layers of “safety” no longer make patients safer.
Sometimes the hardest thing in medicine is to recognize when we’ve reached “good enough.”
References:
- Lalonde, D., Martin, A., & Bell, M. (2012). Wide-awake flexor tendon repair and early tendon mobilization in zones I and II. Journal of Hand Surgery (European Volume), 37(10), 919-924. PubMed
- Clarkson, J. (2024). Infection Rate Comparison during Transition from Hospital Operating Room to Office-Based Procedure Room for Hand Surgery. Full Text
- Avoricani, A., et al. (2021). WALANT Hand and Upper Extremity Procedures Performed With Minor Field Sterility Are Associated With Low Infection Rates. Plastic Surgery, 30(122-129). Consensus
- Yu, J., et al. (2019). Evidence-based sterility: the evolving role of field sterility in skin and minor hand surgery. Plastic and Reconstructive Surgery Global Open, 7. Consensus