Enhancing Patient Care Through Office-Based Surgery at Heritage Hand and Plastic Surgery
One of the key missions at Heritage Hand and Plastic Surgery is to provide patients with the option to avoid Ambulatory Surgery Centers (ASCs) or hospital outpatient departments for procedures that can be safely and efficiently performed in our office procedure room. While we’re not the only practice offering this service in the US, it’s still very, very rare, less than 4% of suitable hand surgery is even offered in the office at all.. Let me explain why this matters.
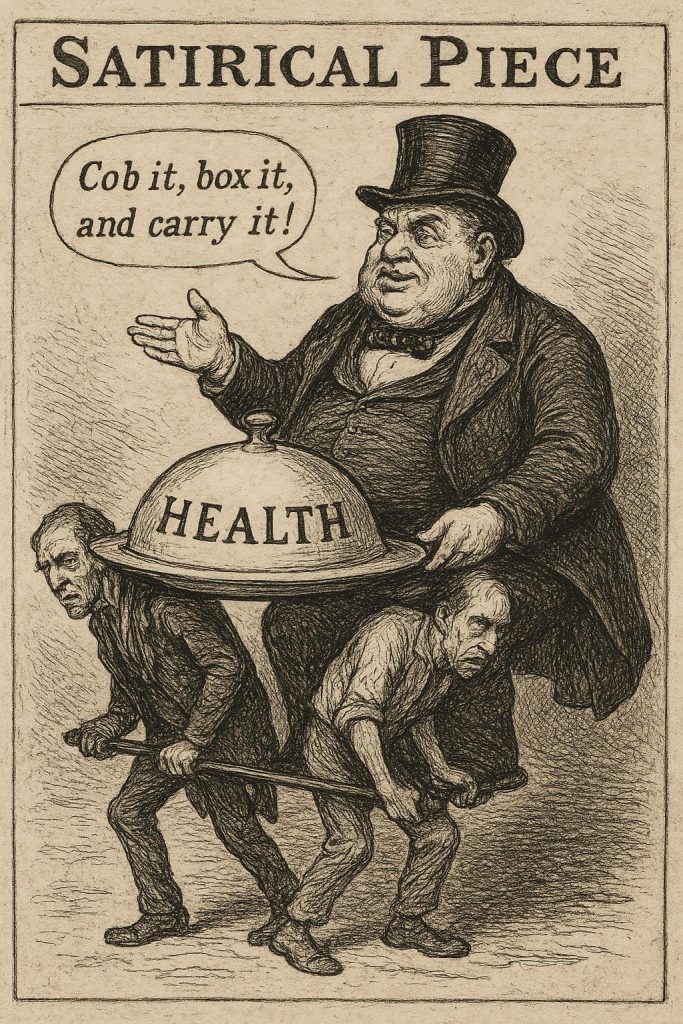
We all pay for health insurance in one way or another—through premiums, taxes via Medicare and Medicaid, or employer-sponsored plans where employees contribute varying amounts through payroll deductions and added premiums. Since the rising cost of healthcare is a critical factor, prudent patients expect their money to be used efficiently. Unfortunately, that’s often not the case. Having worked in the British National Health Service for 13 years before moving here, the differences are stark.
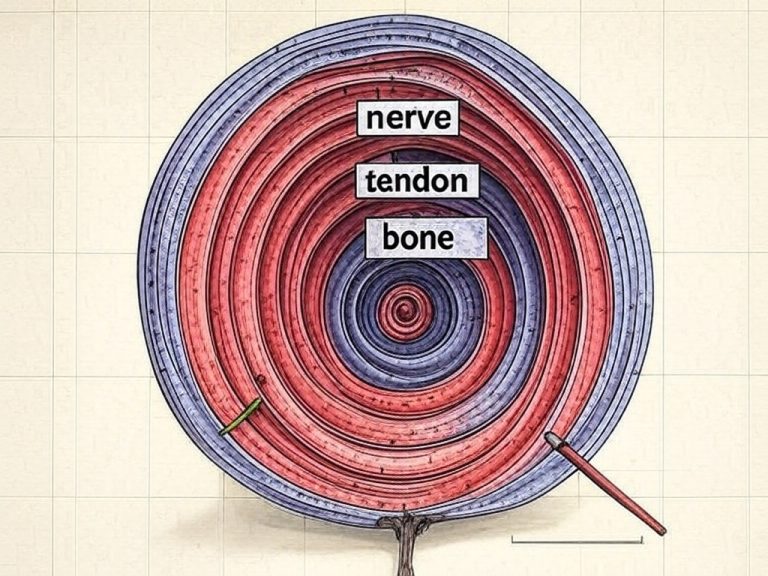
Consider a frail 85-year-old Medicare patient who needs surgery for Cubital Tunnel Syndrome—a common condition where the ulnar nerve (which can cause hand wasting and pain) becomes trapped behind the “funny bone” at the elbow. Proven methods exist to decompress this nerve under local anesthesia in an office setting, and I’ve performed hundreds of these procedures successfully. Yet, Medicare patients are often told that the “site of service” must be a main operating room, not an office procedure room. Why force them into a more complex environment?
You might assume traveling to another location is no big deal, but that’s overlooking a key issue: Most ASCs and hospitals don’t routinely offer fully awake procedures. Their standard protocols lean toward general anesthesia or sedation. For an elderly patient, this means preoperative labs, chest X-rays, EKGs, and clearances from cardiology or pulmonology—requiring multiple trips and appointments. What could be a simple one-hour office visit turns into half a dozen errands, numerous phone calls, fasting from midnight (leading to dehydration), skipping usual medications, and arranging transportation to and from the facility.
Moreover, there’s growing concern that central nervous system anesthesia—whether light or deep—can lead to postoperative confusion and potential long-term cognitive effects. It’s a significant burden to funnel all patients through this “maximalist” system when simpler alternatives like local anesthesia and office-based surgery are available.
We’ve been offering these services for four months now, but not a single insurance company or health payer has helped cover the extra expenses associated with hosting office surgeries. There’s a regulatory barrier at play: the Certificate of Need (CON), which in most states is treated like a liquor license—issued sparingly and rarely surrendered. Local hospitals and ASCs guard their CON status fiercely, allowing them to charge 10-20 times the surgeon’s fee for “supersized” services that aren’t always necessary. Don’t misunderstand me, when you need that level of care in the US, it’s world class, and very designed.
It’s time to rethink, reset, and innovate. Through a company I co-founded called WSS, I’ve been working with communities across the US to encourage surgeons to perform more procedures in their offices. This hinges on site-neutral payments that follow the patient. If office-based surgery costs far less, the facility fee should be reduced accordingly—but at minimum, it should cover costs and incentivize a top-down recalibration of how we, as a nation, choose to spend our healthcare dollars.
In the meantime, my “experiment” continues here in Lansing, where I continue to offer awake surgery wherever possible in the office setting, making use of immersive technology to make the whole process fun and engaging for my patients, whilst remaining safe and economically lean.